Dr. Ramirez attended medical school at the Universidad Autonoma of Guadalajara School of Medicine in Guadalajara Mexico. Dr. Ramirez performed his Neurosurgery training at the National Institute of Neurology and Neurosurgery in Mexico City

Cervical discectomy and fusion is a surgery to remove a degenerative or herniated disc in the cervical spine. An incision is made in the neck to access to the front of the spine. After the disc is removed, a graft is implanted to fuse together the bones above and below the disc. Cervical fusion surgery is indicated if physical therapy or medications fail to relieve your neck or arm pain caused by compression of the spinal cord or spinal nerves.
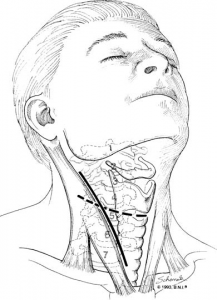
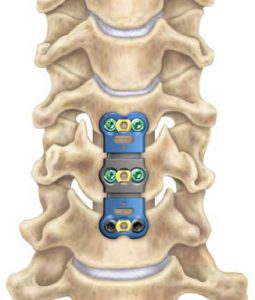
Figure 1. Approach for cervical discectomy and fusion
Discectomy means “removing the disc.” A discectomy can be performed anywhere along the spine. In the cervical spine, the surgeon usually reaches the damaged disc from the front of the spine through the throat area. The neck muscles are retracted and then the trachea, esophagus, the disc, and bony vertebrae are exposed (Figure 1). Surgery from the front of the neck is much more accessible than from the back because the disc can be reached without damaging the spinal cord. Depending on your particular symptoms and findings of magnetic resonance, one disc or more may be treated.
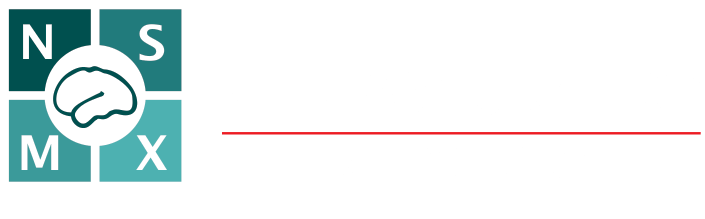
After discectomy, the space between the bony vertebrae is empty. To prevent the vertebrae from collapsing and rubbing together, a bone graft is inserted to fill this space. The graft acts as a bridge between both vertebrae to promote a spinal fusion. The bone graft and vertebrae are usually fixed in place with titanium screws and plates. Following surgery, the body begins its natural healing process, and new bone cells grow around the graft. After 3 to 6 months, this graft should join the two vertebrae and form one solid piece of bone. The hardware and graft work together, similar to reinforced concrete.
There are different sources of bone grafts. Each type has pros and cons.
If more than two levels are fused, you may notice some limitation in turning your head and looking up and down. Motion-preserving artificial disc replacements have emerged as an alternative to fusion. Similar to knee replacement, the artificial disc is inserted into the damaged joint space and preserves motion, whereas fusion eliminates motion. Outcomes for artificial disc compared to ACDF are similar, but long-term results of motion preservation and adjacent level disease are not yet proven. Talk with your surgeon about whether ACDF or artificial disc replacement is most appropriate for you.
You can be a candidate for discectomy if you have:
Cervical fusion could be helpful to treat these conditions:
Bulging and herniated disc: The gel-like material within the disc can bulge or rupture through a weak area in the disc wall. Nerve or spinal cord compression causing neurological symptoms may occur.
Degenerative disc disease: All discs naturally wear out, leading to bone spurs formation and inflammation of facet joints. The discs lose water, dry out and shrink, losing their flexibility and cushioning properties. The disc spaces get narrower. These changes lead to canal stenosis or disc herniation.
Most herniated discs heal after a few months of conservative treatment. Your physician may recommend different treatment options, but only you decide whether surgery is right for you. Be sure to consider all the risks and benefits before making your decision. Only 10% of people with herniated disc problems have enough pain after 6 weeks of conservative, these patients should consider surgery.
Your surgeon will also discuss the risks and benefits of different types of bone graft material. Autograft is the gold standard for rapid healing and fusion, but the hip incision can be painful and at times lead to complications. Allograft is more frequently used and has proven to be effective for routine 1 and 2 level fusions (Figure 2).

Figure 1. Approach for cervical discectomy and fusion
A trained neurosurgeon or an orthopedic surgeon can perform spine surgery. Many spine surgeons have specialized training in complex spine surgery. Ask your surgeon about their training, especially if your case is complex or you have had previous spinal surgeries.
Cervical discectomy is successful in relieving arm pain in 90 to 100% of patients. However, arm weakness and numbness may persist for several weeks. Neck pain is relieved in 70 to 80% of cases. Typically, people with arm pain benefit more from cervical discectomy than those with neck pain.
Achieving a spinal fusion varies depending on the technique used and your general health. A study that compared two techniques: cervical fusion with or without the use of screws and plates, the outcomes were:
93% of people who underwent cervical fusion with bone graft placement achieved fusion.
100% of people who underwent cervical fusion with bone graft placement and plates and screws achieved fusion.

Dr. Ramirez attended medical school at the Universidad Autonoma of Guadalajara School of Medicine in Guadalajara Mexico. Dr. Ramirez performed his Neurosurgery training at the National Institute of Neurology and Neurosurgery in Mexico City

Dr. Ramiro Pérez attended medical school at the University of Guadalajara School of Medicine in Guadalajara México. Dr. Pérez performed his Neurosurgery training in Centro Medico Siglo XXI IMSS and has been practicing his specialty for more than 13 years.

Dr. Nares attended medical school at the University of Aguascalientes, He is trained to perform anterior and lateral approaches to the spine from the cervical to the lumbar spine, as well as minimally invasive surgery.

Dr. Luis Robles has been practicing neurosurgery specialty for 20 years. Dr. Robles is academically active, he participates as a section editor in the World Neurosurgery journal and he has published several articles in different neurosurgery international journals.