Surgery For Chiari Malformations
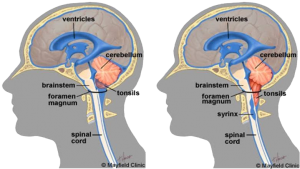
Figure 1. Approach for cervical discectomy and fusion
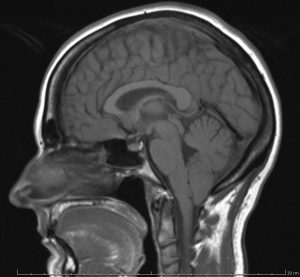
Chiari malformation (CM) is an anomaly in which the lower part of the brain called the cerebellum extends into the spinal canal. Normally, the cerebellar tonsils are located just above the foramen magnum. However, in individuals with Chiari, the tonsils hang below the foramen magnum and herniate into the spinal canal (Figure 1). The degree to which the tonsils extend can vary tremendously.
Chiari malformation is uncommon, but increased use of imaging tests have led to more frequent diagnoses. Chiari malformation is categorized into several types, depending on the anatomy of the brain tissue that is displaced into the spinal canal, and whether developmental abnormalities of the brain or spine are present. The most common type is Chiari I malformation which this article addresses.
Chiari malformation type I develops as the skull and brain are growing. As a result, signs, and symptoms may not occur until late childhood or adulthood. The pediatric forms, Chiari malformation type II and type III, are present at birth (congenital).
Treatment of Chiari malformation depends on the form, severity and associated symptoms. Regular monitoring, medications, and surgery are treatment options. In some cases, no treatment is needed.
Symptoms
Many people with Chiari malformation have no signs or symptoms and do not need treatment. Their condition is detected only when tests are performed for unrelated disorders. Others may have symptoms such as:
- Headache
- Neck Pain
- Dizziness
- Unsteadiness
- Poor coordination
- Vision Problems, Double or Blurred vision
In some patients, Chiari malformation is associated with other neurological disorders including
- Hydrocephalus. It is an accumulation of excess fluid within your brain which may require placement of a flexible tube (shunt) to divert and drain the cerebrospinal fluid to another area of your body.
- Spina bifida. Spina bifida is a condition in which the spinal cord or its covering is not fully developed. In these cases, a part of the spinal cord is exposed, which can cause serious conditions such as paralysis. People with Chiari malformation type II usually have a form of spina bifida called myelomeningocele.
- Syringomyelia. Some people with Chiari malformation also develop a condition called syringomyelia, in which a cavity or cyst (syrinx) forms within the spinal column.
- Tethered cord syndrome. In this condition, the spinal cord attaches to your spine and causes the spinal cord to stretch. This can cause severe nerve and muscle damage in the legs.
Diagnosis of Chiari Malformation
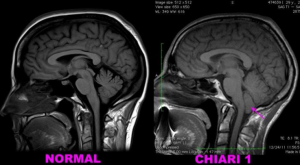
Fig 2 MRI displaying a healthy patient left and another with Chiari malformation. Note the descend of cerebellar tonsils into the spinal canal.
To diagnose your condition, your doctor will review your medical history and symptoms and conduct a physical examination.
Your doctor may order imaging tests to determine the cause of your condition and diagnose your disease. The best test to evaluate patients with Chiari malformations is the MRI.
–Magnetic resonance imaging (MRI). An MRI is often used to diagnose Chiari malformation (Figure 2).
An MRI can be repeated over time, and it can be used to monitor the progression of the disorder.
Treatment of Chiari Malformation

Fig 3. MRI, pre and postoperative changes.
Treatment for Chiari malformation depends on the severity and the characteristics of the condition. If you have no symptoms, your doctor likely will recommend no treatment other than monitoring with regular examinations and MRIs. If symptoms are mild and not progressing, your doctor may recommend conservative management. Supportive care such as a headache and pain management, physical therapy or a reduction in activities can help manage symptoms.
When symptoms do not improve, surgery may be considered as an option.
In the most common surgery for Chiari malformation, called posterior fossa decompression, your surgeon removes a small section of bone in the back of your skull, relieving pressure by giving your brain more room (Figure 3). In some cases, the surgeon may also remove a small portion of the spinal column to relieve pressure on your spinal cord and allow more space for the spinal cord. The specific surgical techniques will vary among surgeons; no consensus yet exists on the best variation on this surgical procedure.
Awesome Doctors for your Neurosurgery Needs

Dr. JJ Ramirez
Neurocirujano
Dr. Ramirez attended medical school at the Universidad Autonoma of Guadalajara School of Medicine in Guadalajara Mexico. Dr. Ramirez performed his Neurosurgery training at the National Institute of Neurology and Neurosurgery in Mexico City

Dr. Ramiro Pérez
Neurosurgeon
Dr. Ramiro Pérez attended medical school at the University of Guadalajara School of Medicine in Guadalajara México. Dr. Pérez performed his Neurosurgery training in Centro Medico Siglo XXI IMSS and has been practicing his specialty for more than 13 years.

Dr. Felipe Nares
Neurosurgeon
Dr. Nares attended medical school at the University of Aguascalientes, He is trained to perform anterior and lateral approaches to the spine from the cervical to the lumbar spine, as well as minimally invasive surgery.

Dr. Luis A. Robles
Neurosurgeon
Dr. Luis Robles has been practicing neurosurgery specialty for 20 years. Dr. Robles is academically active, he participates as a section editor in the World Neurosurgery journal and he has published several articles in different neurosurgery international journals.